-
Diabetic Foot Care: Importance, Tips, and Warning Signs
posted: Apr. 07, 2024.

-
Symptoms of an Ingrown Toenail
posted: Apr. 01, 2024.

-
Treating Plantar Fasciitis
posted: Mar. 12, 2024.

-
Managing Your Heel Pain
posted: Mar. 01, 2024.

-
The Role of Podiatry in Managing Foot and Ankle Fractures
posted: Feb. 07, 2024.

-
What You Need To Know About Ingrown Toenails
posted: Feb. 01, 2024.

-
Sports Podiatry: Addressing Foot and Ankle Injuries in Athletes
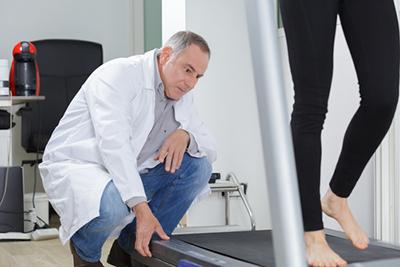
posted: Jan. 07, 2024.

-
Orthotics and Their Role in Foot Health: Custom Solutions for Various Conditions
posted: Jan. 01, 2024.

-
Diabetic Foot Care: Preventing Complications and Maintaining Foot Health
posted: Dec. 07, 2023.

-
Preventing Foot Injuries: Tips for Proper Foot Care and Injury Avoidance
posted: Dec. 01, 2023.

-
The Benefits of Seeing a Podiatrist
posted: Nov. 07, 2023.
-
The Benefits Of Orthotics
posted: Nov. 01, 2023.

-
When To See a Podiatrist
posted: Oct. 06, 2023.

-
The Importance of Diabetic Care
posted: Oct. 01, 2023.

-
Diabetic Foot Ulcers: Effective Treatment Strategies in Colorado Springs
posted: Sep. 15, 2023.
Diabetes, a chronic condition affecting millions of Americans, can lead to many complications if not managed properly. One such complication that often goes overlooked but can be particularly debilitating is Read more -
Treating Your Bunion Symptoms
posted: Sep. 13, 2023.

Our Location
Find us on the map
Hours of Operation
Our Regular Schedule
Monday:
8:00 am-5:00 pm
Tuesday:
8:00 am-5:00 pm
Wednesday:
8:00 am-5:00 pm
Thursday:
8:00 am-5:00 pm
Friday:
8:00 am-5:00 pm
Saturday:
Closed
Sunday:
Closed
